
The weekend of April 18, three people died while staying in Manhattan’s Hilton Garden Inn on 37th Street, one of the hotels participating in New York City’s program to make rooms available for people who tested positive for the coronavirus or are symptomatic.
The purpose of the city’s hotel program is to provide places for people to isolate without spreading the virus to other members of their households. Rooms have also been made available for some individuals who are homeless and health care workers who are frequently in contact with patients, so they can avoid exposing their family members at home.
While the use of hotels as isolation facilities can be an effective weapon against the spread of the virus, the method also poses challenges for consistent monitoring of people’s health and safety while staying in commercial hotels.
In response to the deaths at Garden Inn, Mayor Bill de Blasio promised during Thursday’s coronavirus briefing to increase the clinical staffing at hotel facilities.
“There was a monitoring process in place,” de Blasio said, “but based on this experience, we’re going to be … having clinical personnel monitoring people regularly in these sites to make sure that folks are safe, even if they appeared to be fully and appropriately discharged.”
According to the mayor’s office, the city is making changes to the hotel program for COVID positive or symptomatic individuals. For example, they are adding 24/7 staff on-site beyond the existing hotel staff and they’re going to hire a new official to oversee the hotel program. NYC Health + Hospitals medical staff has assessed all guests at the Hilton Garden Inn. The mayor’s office said the H+H staff will assess all guests in other hotels within the city’s program by the end of this Thursday and decide whether to transfer people to a higher-level of care if needed. They’re also reviewing the criteria for entering people into isolation hotels.
The situation — at least prior to the city implementing these new changes — put a significant responsibility in the hands of hotel staff. The question is how much support and oversight has New York City been giving hotels?
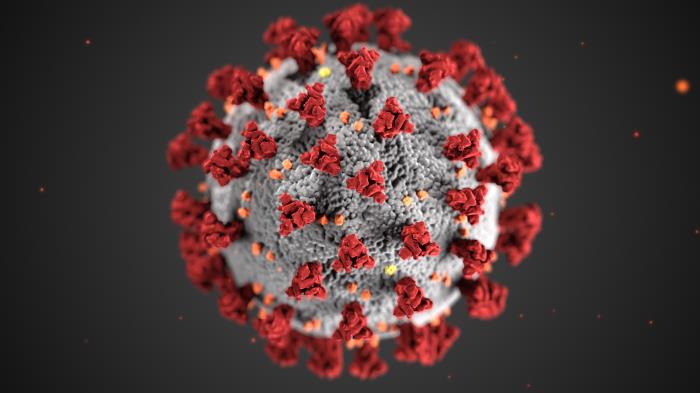
What’s certain: We’re not certain of much about COVID-19
In the mayor’s comments Thursday, de Blasio seemed to suggest that the prospect of someone dying from coronavirus after being discharged from the hospital was unexpected. He said, “You’d think if someone has been discharged from the hospital, it’s an all clear and the reason they’re in a hotel is simply transitional.”
From the very beginning, public health experts emphasized the uncertain and confusing nature of how coronavirus affects patients, since it’s a virus the world had never seen before. In fact, infectious disease specialists still have questions about the nature of COVID-19 today.
As early as a month ago, Michelle Gong, the director of critical-care research at Montefiore Medical Center in the Bronx, told viewers that she was seeing “surprises” over the course of her team treating patients with coronavirus, in an interview with JAMA Network, which publishes The Journal of the American Medical Association. Doctors across the country have been saying that they’ve seen cases in which people feel better for some time and then, their condition deteriorates rapidly.
The physicians’ experiences treating coronavirus patients highlight the value of consistent monitoring, especially for people who have confirmed cases of the coronavirus.
A SUNY Downstate Medical Center representative says health agencies are really the ones responsible for the safety of coronavirus patients if they’ve already been discharged from the hospital and are in isolation facilities arranged by the government, such as hotels.
The challenges of staying open
Margaret Sowa is the general manager of Hotel Le Bleu, a boutique hotel in Brooklyn that’s still open and offers emergency workers discounted rates. Hotel Le Bleu isn’t housing people who have tested positive for the coronavirus. But according to Sowa’s knowledge in speaking with others who work in hotels around the city, even before the changes announced by de Blasio last week, New York City had been requiring that individuals who are COVID-positive or symptomatic receive two “wellness checks” by phone if they are isolating in hotel rooms.
Especially during the early days of New York City’s public health crisis, Sowa says it was extremely difficult to purchase cleaning supplies and disinfectants. When she tried to buy the materials she needed for Hotel Le Bleu to remain open in accordance with public health guidelines, Sowa was told hospitals and nursing homes were getting priority.
She ended up procuring the necessary disinfectants and supplies through connections in the hospitality cleaning industry that she had formed over the course of her career. At the beginning of the crisis, however, Sowa felt she didn’t have a choice but to accept when people drove around offering to resell cleaning supplies at prices inflated around 50 percent greater than usual.
“If I were unable to get crew cleaning and protective gear, I would not stay open. No business is worth endangering human life,” Sowa says.
Like Hotel Le Bleu, The Roosevelt Hotel in Midtown is offering rooms for essential employees like healthcare workers at discounted rates. The hotel’s general manager Marc Sternagel says, “The biggest struggle is the uncertainty.”
He says it’s been a difficult decision for hotels to determine whether to stay open and offer rooms for people who have not tested positive for COVID-19, to figure out how to work with the city to provide rooms for people in isolation after testing positive, or to close down. For the hotels that stay open, it’s a challenge to shift away from the customer-service focus of hospitality towards the priority today, which is primarily the health and safety of employees and guests.
When asked about how The Roosevelt Hotel is monitoring the health of people who come in and out to prevent the virus from spreading there, Sternagel says, “It’s a bit of touchy subject because you need to protect people’s privacy.”
Stan Kennedy, chief operating officer of Remington Hotels, which manages Embassy Suites in Times Square, expressed similar sentiments. “The protocol of testing temperatures of everyone who enters the hotel still needs to be considered,” Kennedy says. “Placing requirements like these are counterintuitive to the art of hospitality but with the severe impact and threat that this virus has introduced, we, as all in the industry, will be required to find that new balance between hospitality service and proper health and safety practices.”
Sternagel says that while “before, hotels were a place of assembly,” now people are staying away from each other. The essential workers who stay at The Roosevelt Hotel, he says, have been following public health guidance like wearing masks, frequent hand-washing, and maintaining six feet of distance from others because they’re also concerned about their health and safety.
Many of the guests who haven’t tested positive for coronavirus are still in contact with people who have the virus, through their work in emergency services and healthcare sectors. That’s why Sowa says Hotel Le Bleu treated the situation as if they did have guests with the virus, implementing cleaning procedures that take place hourly.
“We don’t know who people interacted with. We’re using disinfectants after every interaction,” says Sowa. “We have to protect them, we have to protect us, and everyone who comes through the hotel.”
Concerns persist about resources
Prior to the public health crisis, New York City had already used commercial hotels to house families who are homeless. With more and more services accessible online rather than in-person, the Citizens’ Committee for Children of New York (CCC) has raised concerns about the increased isolation these families face.
Raysa S. Rodriguez, CCC’s associate executive director for policy and advocacy, says, “One of the things that this public health crisis is pointing to is the privilege of having technology and access to affordable digital services. With this pandemic, everything has gone remote — from work to learning to benefits.”
She raises the question, “What happens to those who lack internet and technology?”
Rodriguez says even before the current public health crisis, there was concern about placing families in commercial hotels that lack the laundry facilities, kitchen capacity, and kid-friendly recreational activities.
Advocates for the homeless like VOCAL-NY, Human.nyc, and the Safety Net Project of the Urban Justice Center have spoken out about their concerns regarding the need for greater assistance to New Yorkers who are homeless and have been able to access the city’s hotel program. These concerns surrounded the need for social services to be made clearly known and available. Organizers from these groups have also raised concerns regarding the potential risks posed by placing strangers in hotel rooms together without social services staff within arm’s reach.
A representative from New York City’s Department of Social Services confirmed that they’re placing two people in one hotel room in some cases.
VOCAL-NY homelessness union organizer, Celina Trowell says, “We want to ensure people are linked to care to help them survive the process. Again, it’s a traumatic time. We know that isolation can increase mental health concerns.”
Nicole Javorsky is a Report for America corps member.









2 thoughts on “Hotels as COVID Convalescent Homes: Challenges for Patients, Staff”
By what legal authority is NYC placing recovering covid-19 patients in these hotel rooms? What is the city paying the hotels involved?
NYC Emergency Management is in charge of this program. Crew Facilities won the city’s contract to handle COVID-related hotel stays which was then subcontracted to Hotel Engine. They are paying hotels up to $235/night and the worst part… Crew Facilities/Hotel Engine’s commission is $30-40 PER NIGHT. Think about how much taxpayer money the city is throwing out the window to an out of state contractor. There are no words to justify the city’s mismanagement of funds.
https://www.thecity.nyc/coronavirus/2020/5/25/21270824/texas-firm-reaps-millions-booking-covid-hotel-rooms-for-nyc